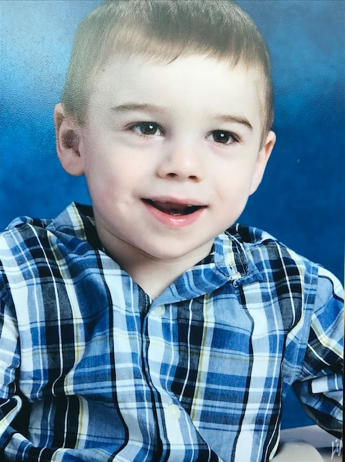
Claire’s Legacy: Inspiring Hope in the Face of the Unknown

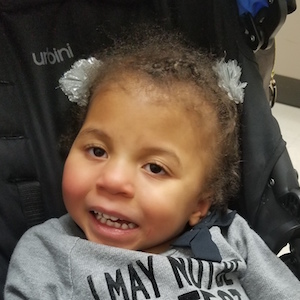
After a healthy pregnancy and easy delivery, our first daughter and second child, Claire, was born on November 4, 2023 at 8:49 AM. Everything seemed fine. She had her first evaluation by the neonatologist and breastfed 6 times between her birth and 3:00 PM. Around 4:00 PM, our mother baby nurse just came into our room to check vitals and give Claire her first bath. That’s when we noticed her very first episode. It looked like she could have been choking, but she was holding her breath and turning blue. When the nurse couldn’t get her to breathe on her own, she was rushed to the NICU and hooked up to oxygen. She had a few more episodes like this and was admitted to the NICU. Claire remained in St. Tammany Parish Hospital for 5 days, in a level 1 NICU, until her breathing got worse and she was transferred to Ochsner Baptist Hospital in New Orleans, where she was first intubated because they were no longer able to control her episodes. About 22 hours later, Dr. England, Ochsner Baptist Medical Director of the NICU, believed that Claire suffered from an unknown metabolic disease and had us transferred again to Children’s Hospital New Orleans to be under the care of Dr. Hans Anderson, Louisiana’s top genetic specialist. Many tests were done at Children’s Hospital. “At one point, 2 of 4 UOA have had significant amount of 3methlyglutaconic acid and 3-methylglutaric. When the Rapid Whole Genome to Gene DX came back entirely negative, Dr. Anderson had to re-look at 3MGA genes for VUS’s, etc. Nothing was found.”

Claire had her ups and downs while at Children’s Hospital. At one point in mid-December 2023, she was well enough for discharge, but she could not pass the swallow study, so we elected for a gastrostomy tube surgery so we could bring her home. Just a week later, she tested positive for COVID. Although she did not have any symptoms, her heart function deteriorated after she contracted this virus. On December 31, 2023, she had to have emergency surgery for pericardial effusion to remove fluid around her heart. The cardiac surgeon put a pericardial window and chest tubes to drain any excess fluid.
She passed away on January 29th, 2024, a few days shy of 3 months, in her parents’ loving arms. Claire’s side effects of this unknown metabolic disease include an enlarged heart, hypertrophic cardiomyopathy, pericardial effusion, elevated lactates, bilateral hearing loss, bilateral cataracts, and irregular brain function as shown on an EEG.
Our hope is that Claire’s story will be able to inspire others to never give up hope during difficult times, continue the search of answers of the unknown and eventually diagnose Claire’s disease, and help others who may suffer from this disease with a cure one day. Claire lived for a wonderful 87 days that we cherished so greatly; now we hope her legacy will live on forever with the help of each of you.
— Michael and Toni Guasco















































































































































































 Thank you again to the Smith family for sharing their words of wisdom with the UDN! To hear more from Chad the Dad, click
Thank you again to the Smith family for sharing their words of wisdom with the UDN! To hear more from Chad the Dad, click